Common medications cause long-term gut changes, study finds, with effects persisting for years after use
10/06/2025 / By Cassie B.
- Nearly 90% of common medications cause lasting changes to your gut bacteria.
- These microbial changes can persist for more than three years after stopping treatment.
- Effects accumulate with higher doses and longer durations of use.
- Many non-antibiotic drugs, like those for anxiety, reshape the gut as much as antibiotics.
- Diet is the strongest driver for recovery, with a high-fiber diet being crucial.
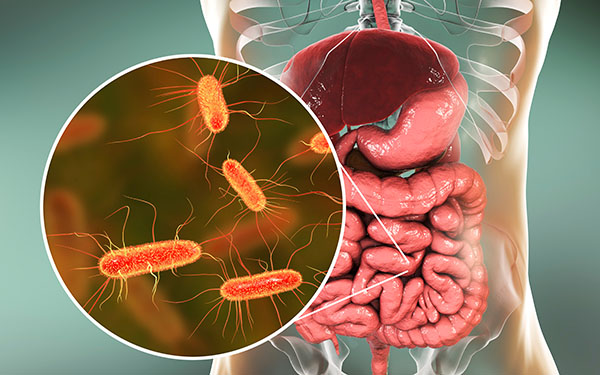
You might think your body fully recovers after you stop taking a medication, but groundbreaking new research reveals your gut remembers everything. A comprehensive study from the University of Tartu has uncovered that nearly 90% of commonly prescribed medications—including those for blood pressure, anxiety, and stomach acid—leave lasting changes to your gut bacteria that can persist for years after you’ve stopped taking them.
The study, published in mSystems, analyzed prescription records and gut microbiome data from more than 2,500 participants in the Estonian Biobank. Researchers discovered that the effects weren’t limited to antibiotics, which are known to disrupt gut health. Drugs targeting human cells—including antidepressants, beta-blockers, proton pump inhibitors, and benzodiazepines—similarly reshaped gut microbial composition in ways that outlasted the treatment period.
Lasting microbial fingerprints
Perhaps most alarming was how long these changes persisted. The research team found that medications left microbial “fingerprints” still visible more than three years after people had stopped taking them. Dr. Oliver Aasmets, the study’s lead author, noted that “past drug use can be just as important as it is a surprisingly strong factor in explaining individual microbiome differences.”
The study revealed that these effects accumulate over time. Higher doses and longer durations of use created stronger, longer-lasting shifts in the microbiome. This additive pattern was observed with benzodiazepines, steroids, and beta-blockers, meaning that the more frequently and longer you take these medications, the more profound the impact on your gut health.
Beyond antibiotics
While antibiotics have long been known to disrupt gut bacteria, the study found that other drug classes created similar patterns. Benzodiazepines, commonly prescribed for anxiety, changed the gut as much as certain broad-spectrum antibiotics by reducing microbial diversity. Antidepressants also left patterns similar to those seen with antibiotics.
Nutritionist Kara Siedman, who wasn’t involved in the research, explained that “We often think of medications as acting only on human cells, but they also interact with the gut ecosystem—the microbes, the intestinal barrier, and the immune system.”
The research identified particular bacterial families affected by medication use. The Clostridium family increased with exposure to antidepressants and beta-blockers—some species of which are linked to rare infections in humans. Benzodiazepines were associated with increases in Dorea formicigenerans and Ruminococcus torques, bacteria linked to obesity, metabolic syndrome, and gut conditions like Crohn’s disease.
Even within the same drug class, different medications had varying impacts. For example, the anti-anxiety drug alprazolam (Xanax) led to a greater loss of gut microbial diversity than diazepam (Valium), suggesting that some medications might be gentler on gut health than others treating the same condition.
Recovery and resilience
The good news is that recovery is possible, although it is not always complete. Diet emerged as the strongest driver of microbiome health and resilience. Siedman emphasized that “what we eat shapes microbial diversity, fiber fermentation, and bile acid production, all of which interact with drugs.”
A high-fiber diet helps restore balance after antibiotic use, while a low-fiber diet can weaken the gut barrier and fuel inflammation, slowing microbiome recovery. The extent of recovery also depends on an individual’s baseline microbiome composition, meaning two people can take the same medication and experience different microbiome shifts and recovery times.
For those requiring ongoing medication, experts recommend practical steps to support gut health: focusing on fiber diversity from whole grains, legumes, fruits, and vegetables; adding polyphenol-rich foods like berries and green tea; including fermented foods like yogurt and kimchi; and considering targeted supplements including probiotics and prebiotics.
This research serves as a crucial reminder that the medications we take today may be affecting our health for years to come, highlighting the importance of avoiding unnecessary medications and supporting gut health through dietary choices.
Sources for this article include:
Submit a correction >>
Tagged Under:
bad medicine, Big Pharma, Censored Science, gut health, gut microbiome, longevity, medical violence, medication, side effects
This article may contain statements that reflect the opinion of the author





















