Obesity causes depression, concludes “strongest evidence yet”
07/25/2019 / By Evangelyn Rodriguez
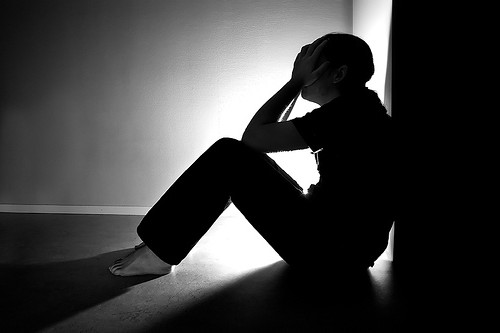
Obesity and depression are global health problems. According to the World Health Organization, an escalating global epidemic of obesity and overweight is taking over many countries. Depression, on the other hand, continues to be the leading cause of disability worldwide. While these diseases affect different aspects of health, several studies have suggested that there is a link between them. In a recent article published in the International Journal of Epidemiology, researchers from the University of Exeter in the U.K. and the University of South Australia (UniSA) Cancer Research Institute show that the psychological impact of obesity, not associated diseases, causes depression in both men and women.
The researchers used a genomic approach…
For their study, the researchers gathered genetic data from the U.K. Biobank, a study conducted from 2006 to 2010 that involved 500,000 individuals aged 37 to 73 years. The researchers looked at data from 48,000 people with depression and compared them to medical and genetic data from 290,000 people born between 1938 and 1971, who served as controls.
The researchers used a genomic approach called Mendelian randomization to test for a causal relationship between depression and having a higher body mass index (BMI). BMI is a measure of body fat based on height and weight and is one of the many tools used to assess a person’s health risks. A BMI greater than 30 kilograms per square meters (kg/m²) is associated with obesity.
The researchers also used self-reported data and hospital data to confirm depression in the participants. In their paper, they wrote: “We used two genetic instruments, both representing higher BMI, but one with and one without its adverse metabolic consequences, in an attempt to ‘uncouple’ the psychological component of obesity from the metabolic consequences.” They also examined causal relationships in men and women separately.

“We separated the psychological component of obesity from the impact of obesity-related health problems using genes associated with higher body mass index (BMI), but with lower risk of diseases like diabetes,” explained Elina Hypponen, a professor at UniSA who co-led the study.
…and found that BMI is linked to risk of depression
The researchers reported that a higher BMI is strongly associated with a higher risk of depression, particularly in women. Their Mendelian randomization experiment provided evidence for this. According to Hypponen, genes that are linked to higher BMI but not to other diseases were just as strongly associated with depression as genes associated with higher BMI and diabetes. This implies that being overweight causes depression, and health issues related to obesity have nothing to do with it.
Additionally, this association is more evident in women than in men. (Related: Magical medical mushrooms? Psychedelics have surprising health benefits, may be next big thing in treating addiction, depression.)
The researchers also explored the relationship between childhood BMI and the development of depression later in life. They asked the participants about their perceived body size when they were 10 years old and found that men and women who perceived themselves as plump at that age had higher odds of reporting depression when they became adults. Similarly, men and women who perceived themselves as thinner than average were also more prone to depression later in life than those who reported being of average weight.
The researchers believe that these could explain the U-shaped relationship between depression and BMI. On the other hand, these results could also be confounded by other factors like poverty.
“The current global obesity epidemic is very concerning,” said Hypponen. “Alongside depression, the two are estimated to cost the global community trillions of dollars each year.”
“Our research shows that being overweight doesn’t just increase the risks of chronic diseases such as cancer and cardiovascular disease; it can also lead to depression.”
Sources include:
Submit a correction >>
Tagged Under:
BMI, body mass index, cardiovascular disease, chronic diseases, depression, diabetes, genomic approach, global health problems, global obesity epidemic, Mendelian randomization, mental health, metabolic consequences, metabolic health, mood disorder, obesity, overweight, Psychology, research, science
This article may contain statements that reflect the opinion of the author